Fertility Awareness
Fertility awareness is an educational process which allows a woman to get in tune with her body by monitoring changes in her menstrual cycle and the indicators of fertility. This allows her to make more informed decisions about her sexual and reproductive health, understand how fertility works and how it is affected by changing circumstances.
Modern fertility awareness methods (FAMs) are based on a scientific and accurate understanding of fertility. These methods can help to optimise chances of pregnancy and, when properly taught using a combination of indicators, offer a highly effective means to avoid pregnancy (Frank-Herrmann 2007)
A basic knowledge of male and female fertility is important for anyone who wishes to understand their fertility - whether for general interest, for planning or avoiding pregnancy.
Male fertility
A man is potentially fertile 24 hours a day seven days a week. For the purposes of fertility awareness we have to assume that a man is producing strong healthy swimmers each time he ejaculates. Sperm can survive in the female reproductive tract for an average of 2–3 days, and potentially for up to a week. Sperm survival is dependent on the secretions at the woman's cervix. These secretions either encourage or block sperm transport, dependent on the phase of the menstrual cycle. The changes in cervical secretions are one of the major indicators (signs) used in FAMs.
Sperm facts
- A man produces sperm on a continuous basis from puberty through to old age.
- At ejaculation, between two and five millilitres of seminal fluid (containing sperm) is released. When first ejaculated, the fluid is thick and sticky (allowing it to stick to the woman’s cervix). After a few minutes it liquefies releasing the sperm to swim through the cervix.
- Approximately 250 million sperm are released at ejaculation, about 30 reach the outer surface of the egg and eventually one sperm will successfully penetrate the egg coat to achieve fertilisation.
- Sperm can survive for an average of 2-3 days, and potentially for up to a week in the female reproductive tract waiting to fertilise the egg.
- Sperm can only progress through the cervical canal when its secretions provide a sperm-friendly transport medium. At other times in the menstrual cycle the cervix is blocked by a thick sticky plug of secretions and sperm are rapidly destroyed by the acidity of the vagina.
- Optimum sperm production requires a consistent temperature that is about 2 degrees centigrade below normal body temperature. Prolonged exposure to excessive heat may be a factor for couples who are trying to conceive.
- Sperm may be contained in the small amount of pre-ejaculatory lubricating fluid, which is released (without warning) prior to ejaculation, so genital contact without full intercourse can result in pregnancy. Withdrawal method (pulling out) is not recommended as a safe contraceptive method.
Female fertility
A woman's fertility works on a cyclical basis. The window of opportunity for conception (the fertile time) averages 9 days during each menstrual cycle. Although the egg can only be fertilised for around 24 hours, sperm can survive in the female reproductive tract for up to a week which means that intercourse on any fertile day could result in pregnancy. A woman can learn to observe her fertility indicators recognising that the fertile time will vary from woman to woman and from one cycle to the next in the same woman.
Egg facts
- A woman is born with her lifetime supply of eggs (approximately 2 million), but the supply is diminishing continuously. By the time a girl has her first period (menarche) at around 12 years old she has around 400,000 egg follicles left.
- A woman releases an egg at ovulation (approximately once a month) from around the time of her first period until she has her final menstrual period (menopause - at around 52 years of age). This means that less than 500 eggs are ovulated throughout reproductive life - the majority are lost through a natural process of degeneration.
- The egg can only be fertilised for around 24 hours. There is always a possibility of a second ovulation (as in the case of non-identical twins) but this always occurs within 24 hours. Total 48 hours is allowed for egg survival.
- Egg quality starts to decline by the time a woman reaches her mid-thirties. This decreases the chances of pregnancy and increases the risk of miscarriage and chromosomal abnormalities such as Down’s syndrome.
- Many women continue to have "periods" long after they have stopped releasing healthy eggs. Regular periods are no guarantee of ovulation.
- The only proof of ovulation is pregnancy. Ultrasound and hormone blood tests provide the strongest evidence of ovulation. Changes in cervical secretions and temperature do not give conclusive proof of ovulation.
- Some women may have a premature menopause (before 40) – this sometimes runs in families. Enquire about any family history of premature menopause.
- Biologically, the ideal time to conceive is 25-35 years.
FIGURE 1: CHANCES OF CONCEPTION BASED ON ESTROGEN AND PROGESTERONE (ADAPTED FROM WILCOX 1995)
The chances of conception
The fertile time in each menstrual cycle (based on hormonal studies) spans 6 days – that is from five days before ovulation to the day of ovulation itself (see figure 1). The time a woman perceives she is fertile, however, averages around 9 days because the indicators of fertility are less precise (and margins of safety are required).
The menstrual cycle
The menstrual cycle describes the roughly monthly pattern of menstruation (periods). The length of the menstrual cycle is measured from the first day of one period (first day of a fresh red bleed) until the day before the next period starts. The average menstrual cycle lasts around 28 days, but some women will have cycles which are much shorter or much longer.
Phases of the menstrual (fertility) cycle
The menstrual cycle generally focuses on menstruation as the key event during the cycle, but for the purposes of fertility awareness it is more appropriate to place the emphasis on fertility, so the term "fertility cycle" is often preferred. The fertility cycle can be conveniently divided into the time before ovulation (the pre-ovulation or follicular phase) and the time after ovulation (the post-ovulation or luteal phase). It is not possible to determine the precise time of ovulation using the subjective indicators, fertility awareness aims to identify the full width of the fertile time.
For practical purposes the fertility cycle is divided into three phases:
- the pre-ovulation relatively infertile time (early infertile time)
- the fertile time
- the post-ovulation infertile time (late infertile time)
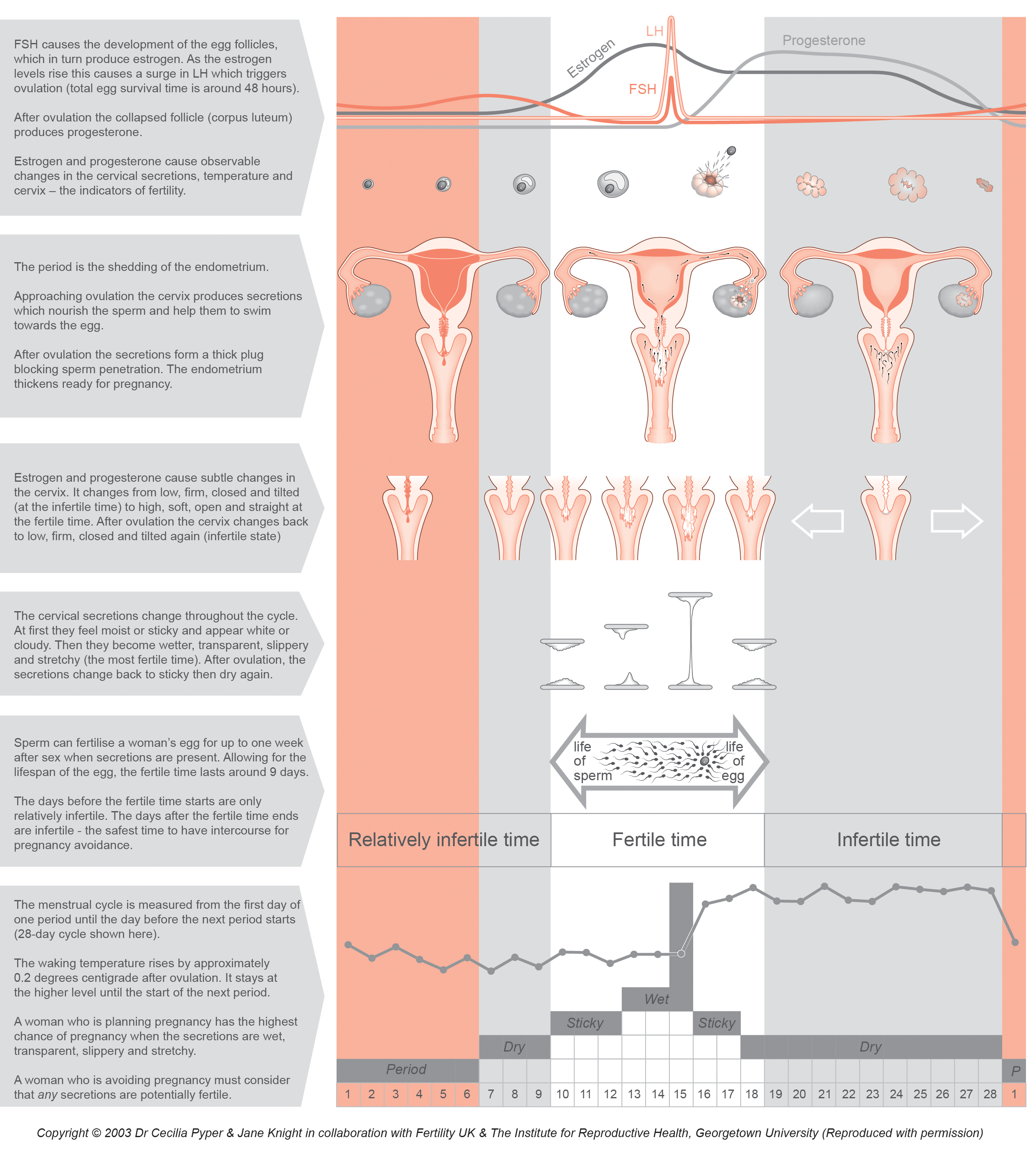
Figure 2 shows a typical 28-day cycle. The pink shading represents the period (shedding of the uterine lining), the grey represents the infertile time (when intercourse is not likely to result in pregnancy) and the white, the fertile time (when intercourse can result in pregnancy). The arrow shows the lifespan of the sperm and egg which together constitute the fertile time.
The post-ovulation phase is constant in length (10-16 days). Once ovulation has been confirmed the rest of the cycle is infertile and there is virtually zero chance of pregnancy. The pre-ovulation phase, however, is more varied in length so is less predictable – ovulation could occur earlier than expected or sperm could survive longer than anticipated – so the time before ovulation is only ever considered relatively infertile.
Sex hormones and their effect on the cycle
The menstrual cycle is under the control of sex hormones. The master gland in the brain (hypothalamus) has overall control and produces releasing hormones, which in turn control the pituitary gland at the base of the brain. In the first part of the cycle, the pituitary produces follicle-stimulating hormone (FSH) which, just as its name implies, stimulates the follicles (containing the eggs) to grow and develop. As the follicles start to grow, they produce increasing amounts of the hormone estrogen. The cervical secretions become wetter, more alkaline and sperm-friendly to encourage the sperm to enter the cervical canal. When the estrogen reaches a critical level it triggers a surge in luteinising hormone (LH) which in turn triggers the release of the egg – this is ovulation.
After ovulation the empty follicle collapses and becomes the corpus luteum or yellow body (named because of its yellowish pigment). The corpus luteum produces increasing amounts of progesterone which thickens the uterine lining (endometrium) in preparation for pregnancy. Progesterone also causes a thickening of the cervical secretions preventing further sperm penetration and a slight rise in waking temperature. The corpus luteum has a fixed lifespan of 10–16 days (average 14 days).
- If an egg has been fertilised it will implant in the endometrium, maintaining the life of the corpus luteum (and the progesterone levels) and triggering the pregnancy hormone hCG (human chorionic gonadotrophin) – this is the start of pregnancy.
- If there is no fertilisation, the corpus luteum degenerates, the progesterone level drops and the next period starts within about 14 days.
Figure 2 summarises the physiological changes which occur during the menstrual cycle. It demonstrates how the ovarian hormones influence the changes in the indicators of fertility. This image can be downloaded for personal use or for teaching purposes from the download area.
Figure 2: The menstrual cycle and the indicators of fertility
Variations in cycle length
The length of the menstrual cycle is measured from the first day of one period (first day of a fresh red bleed) until the day before the next period starts. In a "classic" 28 day cycle, ovulation usually occurs around day 14, but few women consistently have 28 day cycles and this is normal. A variation in cycle length of up to 7 days is still considered regular. The image below shows short, average and long cycles to demonstrate variations in cycle length and the corresponding variation in the position of the fertile time. The time from ovulation to the next period (post-ovulation phase) is around 14 days, so cycle length variation is largely due to the variable length of the pre-ovulation phase.
The fertile time (white block) stays constant at around 9 days (approximately one week for sperm survival and two days for egg survival); so it is easy to see that in a short cycle the fertile time could start during a period. This means that it is quite possible to conceive from intercourse during a period as sperm can survive for up to 7 days waiting to fertilise the egg. In a longer cycle, ovulation will occur much later in the cycle, for example around day 21 in a 35 day cycle. Women using FAMs to avoid pregnancy should keep an accurate record of cycle lengths to allow the use of different calculations to help determine the start of the fertile time.
Figure 3: Variations in cycle length
The indicators of fertility
The major indicators of fertility include the changes in the waking temperature, cervical secretions and cervix, plus calculations based on past cycle length. Minor indicators include mid-cycle (mittelschmerz) pain and breast changes, but these do not correlate closely with ovulation. The indicators of fertility are discussed further in the sections on planning and avoiding pregnancy. The key indicator for women who are planning pregnancy is the changes in cervical secretions. Women who are using FAMs to avoid pregnancy should use a combination of indicators to improve the effectiveness of the method.
Normal cervical secretions or abnormal vaginal discharge?
All women need to be able to distinguish between normal cervical secretions and abnormal vaginal discharge. Normal secretions are white, opaque or transparent - they are odourless. Any discharge which is discoloured, has an offensive odour or is accompanied by redness, soreness or itching should be reported to a doctor promptly. It is not recommended to self-diagnose conditions such as candida (thrush) or to rely on bought medication. Research shows that only about one-third of women who self-diagnosed thrush were correct. Some women had normal swabs about one-fifth of the women had bacterial vaginosis (BV), but others had more serious conditions which could damage fertility. (Ferris 2002)